White Paper
Use
Cases for Social Impact Bonds
in
Schenectady, New York
by Isaac Michaels[1]
Release Date: January 10, 2014
I.
Summary
Social
impact bonds (SIBs) are financial instruments that align incentives in order to
finance socially beneficial preventive interventions using capital from
profit-seeking private investors. In particular, SIBs introduce exciting
opportunities for scaling programs to improve public health. This white paper
discusses how SIBs work, and why they are well suited for public health
applications; it is written in response to a large community health assessment
in Schenectady, New York. The paper proposes four use-cases for SIBs to be
piloted in Schenectady that would reduce incidence of asthma, falls among seniors,
type 2 diabetes, and tobacco smoking. The paper concludes with a discussion
about the future development of SIBs as a new asset class, and recommendations
for Schenectady.
II.
Introduction
Social
impact bonds (SIBs) are an emerging financial instrument for impact investing.
SIBs raise capital from profit-seeking private investors in order to fund
public interventions; appropriate interventions will produce both social impact
and government savings; the performance of the intervention is measured by an independent
evaluator; and, if the intervention achieves predetermined performance
benchmarks, then governments use the resulting savings to repay investors. By
this model, SIBs create opportunities for investors to profit; and, governments
only pay for outcomes successfully achieved.
The
first SIB ever developed was launched in the United Kingdom in 2010. Since
then, others have been piloted. Today, SIBs are being used: to reduce
adolescent recidivism in New York City[2]; to reduce chronic homelessness and to support
youth aging out of the juvenile justice system in Massachusetts[3]; to fund early childhood education in Utah[4]; and to improve asthma morbidity in Fresno,
California[5]. New SIBs are being developed and implemented
throughout the United States, and in other countries.
This
white paper describes SIBs, and how they could potentially be used to improve
public health in Schenectady, New York. In particular, this paper discusses use
cases for SIBs that would scale evidence-based interventions addressing asthma,
falls among seniors, type 2 diabetes, and tobacco smoking. Beyond these
examples, there are many exciting potential applications for SIBs in public
health. I estimate that up to approximately $50 million in averted medical expenditures
and lost productivity could be saved annually by using SIBs in Schenectady to
implement the evidence-based interventions that I will outline.
III.
The Structure of a Social Impact Bond
A
SIB is not actually a bond. A bond is a financial debt instrument in which
investors loan money to a bond issuer, and then the issuer repays investor
principal at a defined interest rate over a set repayment schedule. In
contrast, a SIB is not a debt instrument; it involves a group of contractual
partnerships that finance a socially beneficial project using the resulting
future savings.
The
partnerships that comprise a SIB involve six groups:
1. A
Government
2. An
Intermediary
3. Investors
4. Service
Providers
5. Constituents
6. An
Independent Evaluator
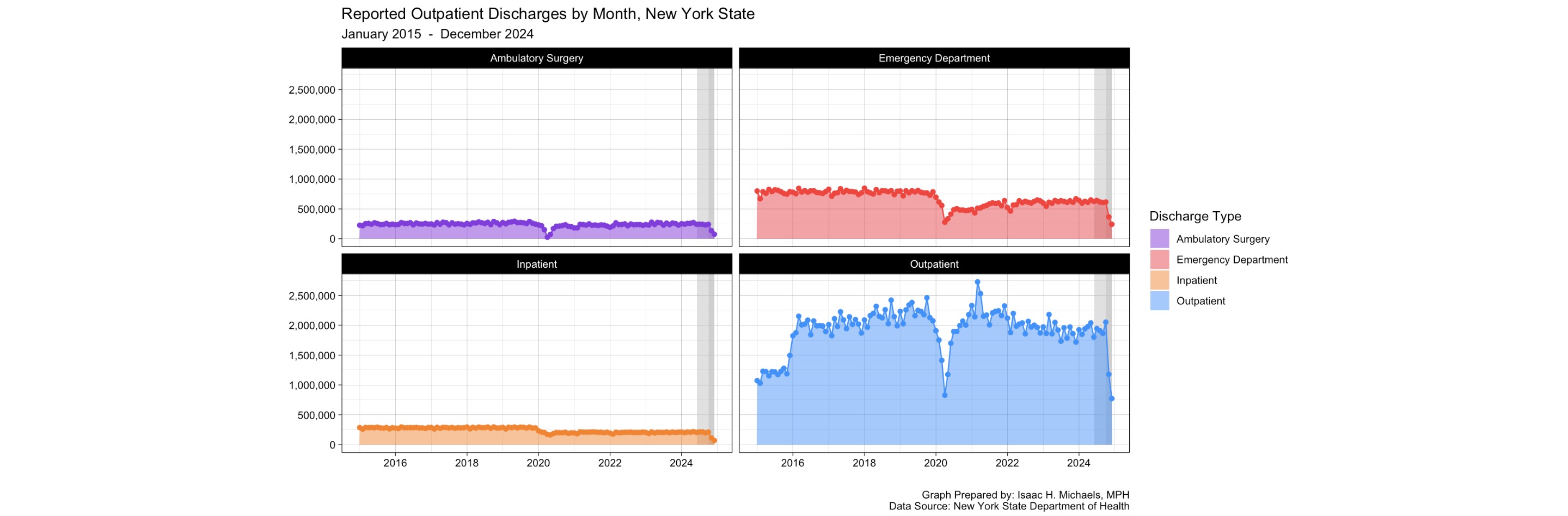
Figure
1 graphically summarizes the interactions between the six groups in a SIB.
The government initiates the formation of a SIB by contracting with an intermediary. The intermediary is tasked with raising capital from investors, and then using the capital to select, finance, and manage one or more service providers. Moreover, the intermediary is the central point of contact between the government, investors, and service providers. The selected service providers use the capital to deliver an evidence-based intervention that creates a positive social impact for constituents; appropriate interventions should generate government savings by using prevention as a means of reducing the size of publicly financed remedial programs. A best practice is to require that participating service providers be invested in the SIB in order to align incentives.
Prior
to raising investor capital, the intermediary works with the government to
define outcomes-based performance benchmarks as objectives for the
evidence-based intervention. Over the lifetime of the SIB, an independent
evaluator periodically measures the performance of the intervention based on
predetermined metrics. The gold standard for measuring the impact of an
intervention is a randomized controlled trial (RCT). RCTs are especially
well-suited for SIBs because they measure the ‘attributable impact’ created by
an intervention as well as the ’total impact’ – which could be the cumulative result of the
intervention and numerous other factors. When a RCT cannot feasibly be
performed, other measurements may be acceptable instead. SIBs can be structured
so that investors receive partial payouts when objectives are only partially
achieved; the success of the intervention at meeting performance benchmarks as
assessed by the independent evaluator would determine the amount of money that
the government gives to the intermediary to pay out to investors. SIBs with
higher rates of return for investors will be able to raise capital more easily;
however, the payout to investors should not exceed the government savings
created by the SIB. A successful SIB should achieve performance benchmarks and
desired outcomes, create government savings, return investor principal, and pay
out to investors a return on capital for taking on risk.
The
emphasis on outcomes is essential. By measuring impact on the basis of outcomes
rather than on units processed, SIBs remove the incentive for service providers
to ‘cherry pick’ the easiest available cases[6]. For example, investors in a SIB designed to
reduce youth recidivism through behavioral counseling should not be compensated
based on the recidivism rate among the children who were counseled; this would
incentivize service providers to only treat the children least likely to
recidivate in the first place. A more appropriate evaluation metric would be
the community-wide rate of youth recidivism; this metric incentivizes service
providers to target the children most likely to recidivate for counseling, and
has the government pay only for successfully achieved community-wide outcomes.
Importantly,
the direct cost-savings that SIBs achieve are not necessarily produced
immediately. A SIB designed to reduce youth recidivism in the juvenile justice
system, for example, will take less time to begin producing cost savings than
will a SIB designed to reduce the incidence of a cancer with a decades-long
latency period. Governments must consider this when developing a SIB, because
they need to include in their budgets capital to pay out to investors.
Governments with poor credit ratings may find when their intermediary raises
capital for a SIB, that investors demand a higher rate of return to compensate
for counterparty risk. If a government is interested in developing a SIB, but
has insufficient capital to pay out investors, then it might consider issuing a
bond. If the present value of the future savings from a SIB is greater than the
cost of paying investors, then a bond can provide governments with capital for
investor payout for SIBs that do not immediately produce government savings.
IV.
Health Impact Bonds
A
SIB that focuses on improving public health is sometimes referred to as a ‘health
impact bond’. The service provider in a health impact bond should deliver a
preventive evidence-based public health intervention that reduces morbidity and
mortality, and thereby creates government savings through averted Medicare
expenditures, Medicaid expenditures, lost productivity, and other public costs.
Health
impact bonds are unique in the sense that the direct savings they create extend
beyond averted government expenditures; by reducing morbidity, health impact
bonds create direct savings for private health insurance providers as well.
This introduces the potential for health impact bonds to be developed by health
insurance companies, either in place of governments, or collaboratively in
partnership with governments. In situations where a public health intervention
could create direct savings for both a government and a private health
insurance provider, the two parties could partner in forming a health impact
bond in which they would divide the responsibility of returning capital to
investors proportionately based on the relative share of the resulting savings
they will experience. For example, consider hypothetically an evidence-based
public health intervention designed to reduce hospitalizations and emergency
department (ED) utilization in a
community by improving access to preventive healthcare; if direct savings
estimates were to suggest that 70% of the savings would benefit the state
government through averted Medicaid expenditures, and 30% of the savings would
benefit a regional health insurance company, then the state government and the
health insurance company could partner in developing a health impact bond by
agreeing to provide 70% and 30%, respectively, of the capital returned to
investors. In certain cases, partnership in a health impact bond could appeal
to both governments and insurance companies; governments would be able to share
the burden of compensating investors; and the cost of capital to be paid out to
investors would be lower for a public-private partnership than it would be for
an insurance company acting independently.
V.
Social Impact Bond Value Proposition
By
aligning incentives, SIBs create opportunities for mutual benefit:
Governments
SIBs
save governments money by replacing remedial programs with preventive intervention.
By engaging private capital, SIBs can mobilize interventions that otherwise
would be unaffordable for governments to finance themselves. Furthermore, by
transferring risk to investors, SIBs enable governments to pay only for
outcomes successfully achieved.
Investors
SIBs
are the growing focus of interest among investors seeking a ‘double bottom-line’
of financial return and positive social impact. Moreover, SIBs represent a new
asset class; it is unlikely that their performance will be correlated with
other investments, and so SIBs may be an appealing solution for certain
investors seeking diversification.
SIBs
may become especially attractive investments for banks. In the United States,
certain SIBs may qualify for CRA credit under the Community Reinvestment Act[7]. This creates opportunities for banks to comply
with the mandates of the Community Reinvestment Act, and yield a financial
return on investment. Investment banks are already responding. Goldman Sachs’ Urban
Investment Group has invested in SIBs in the United States, and intends to
pursue CRA credit[8]; their Urban Investment Group’s GS Social Impact Fund has a target size of $250 million
[9]. In November of 2013, Morgan Stanley announced
the launch of the firm’s Institute for Sustainable Investing[10]; Morgan Stanley has set a five-year goal of
investing $10 billion in impact investments[11].
Constituents
Constituents
benefit directly from SIB interventions. The type and magnitude of benefits
derived are specific to the intervention and target population, and usually
involve both direct and indirect benefits. SIBs can be drivers of job creation
and economic growth in communities; they employ service providers,
intermediaries, and independent evaluators, they can be designed to stimulate
urban renewal, and certain SIBs can direct investment into sustainable
industries and job training programs. Most importantly, SIBs allow innovative
evidence-based interventions to be implemented that could be too novel for
governments to finance themselves with taxpayer funds[12].
VI.
Public Health in Schenectady, New York
Schenectady
is a small city of 66,000 residents in upstate New York, where it is part of
New York’s Capital District[13]. In Schenectady County, the urban city of
Schenectady is surrounded by suburban and rural towns. In 2013, local
organizations were brought together to form the Schenectady Coalition for a
Healthy Community; the coalition was tasked with conducting a community health
assessment, and developing a health-focused community action plan. The
Coalition proceeded by commissioning the UMatter
Schenectady Survey.
The
UMatter survey was a city-wide, neighborhood-level
health assessment administered door-to-door by teams of community health
workers equipped with iPads. The iPads contained up to 283 questions covering a
variety of personal and community health topics. A response-dependent skip
logic programmed into the survey software determined the number of questions
asked of each participant.
Between
February and May of 2013, the UMatter survey
collected 2,074 responses from city residents. Schenectady’s two highest-needs
neighborhoods were intentionally oversampled. The survey’s methods and results
are reported in greater detail in the Coalition’s 2013 Health Needs Assessment
and Community Action Plan, available online[14].
Epidemiologists
analyzed the survey results and reported back to the coalition. Based on the
epidemiologists’ recommendations and analysis, presentations from local
healthcare providers, a voting system, and well defined prioritization
criteria, the coalition members ranked the city’s prevailing public health
issues that most urgently needed to be addressed. The coalition ranked the
following public health issues as the five leading priorities:
1. Mental Health/Substance Abuse
2. Inappropriate Emergency
Department Utilization
3. Teen Pregnancy
4. Diabetes and Obesity
5. Smoking and Asthma (and
Neighborhood Safety)
I
used the findings from the UMatter Schenectady Survey
to assess the suitability for public health-focused SIBs to be implemented in
Schenectady. The following four sections of this white paper outline promising
use cases. Three of the use cases (asthma, type 2 diabetes, and tobacco
smoking) address public health issues that the coalition included in their top
five priorities. One of the use cases (falls among seniors) addresses a public
health issue that the coalition identified as an urgent priority, but did not
include as one of the top five.
VII.
SIB Case: Asthma
Asthma
is especially prevalent among children in urban environments. Below are key
incidence metrics for Schenectady County:
• Asthma ED visits in Schenectady County from 2005-2007 = 3,080 [15]
• Asthma hospitalizations in Schenectady County from 2005-2007 = 637 [16]
From
2005 to 2007, there were an average of 1,026 and 212 asthma-related ED visits
and hospitalizations, respectively, in Schenectady County. The US Census
estimates that in 2012 the city of Schenectady and Schenectady County had
populations of 66,078 [17], and 155,124 [18] respectively. Asthma is often disproportionately prevalent in urban
environments; this suggests that the asthma incidence rate is higher in the
city of Schenectady than in Schenectady county. However, if we assume that
these incidence metrics and demographics are relatively stable, and that the
asthma incidence rate in the city of Schenectady is similar to that of the
county, then we can assume that asthma annually causes approximately 437 ED
visits and 90 hospitalizations in the city.
In
2007, the average cost of an asthma ED visit was $151, and the average cost of
an asthma hospitalization was $6941 [19]. By applying these average costs to our ED visit
and hospitalization estimates, we can estimate that asthma-related
hospitalizations and ED visits in the city of Schenectady annually cost
approximately $690,677.
The
National Cooperative Inner City Asthma Study found that a multi-faceted in-home
tailored intervention was effective at controlling asthma symptoms and reducing
morbidity[20]. This preventive intervention involved home
environmental assessments, education, and, the use of mattress covers, pillow
covers, HEPA vacuums, HEPA air filters, smoking cessation, pest management,
minor repairs, and intensive household cleaning. The study found that, in
children, the intervention lead to a median decrease of 21 asthma symptom days
per year, a median decrease of 12 missed school days per year, and a combined
median decrease of 0.57 acute healthcare visits per year. In adults, the study
found only borderline or no improvement in healthcare utilization.
In
children, the intervention was successful at cost-effectively producing cost
savings through minor or moderate environmental remediation with an educational
component. The cost savings came in the form of averted asthma care
expenditures and improved productivity. For participants who required minor or
moderate environmental remediation, the cost of the program per participant was
between $231 and $3,796; the program cost per participant was $3,796 to $14,858
when major environmental remediation was necessary. Ultimately, cost-benefit
studies determined that the intervention generates $5.30 to $14.00 in return
for every dollar invested.
The
cost-benefit analysis suggests that a SIB would be a sustainable vehicle for
scaling up asthma prevention in the city of Schenectady. Additional study is
still needed beyond these preliminary estimates in order to better understand
asthma-related costs, as well as to better assess the suitability of the multi-faceted
intervention for Schenectady. City-wide asthma-related hospitalization/ED
visits could be good outcome metrics for an asthma-focused SIB.
VIII.
SIB Case: Falls Among Seniors
Schenectady
County experiences a high incidence of falls among seniors, as well as a
fall-related mortality rate that exceeds the New York State average. Below are
three important measures of incidence:
• Mean Annual Frequency of Emergency Department Visits due to Falls in
Residents Ages 65+, 2006-2008 in
Schenectady County = 1,101 [21]
• Mean Annual Frequency of Hospitalizations due to Falls in Residents
Ages 65+, 2006-2008 in Schenectady County = 543 [22]
• Mean Annual Frequency of Mortality due to Falls in Residents Ages
65+,
2006-2008 in Schenectady County = 9 [23]
The
US Census estimates that in 2012, Schenectady County’s ages 65 and older
population was 23,423 [24]. The Census also estimates that in 2012, the city of Schenectady had
a population of 66,078, and that in 2010 11.4% of the city’s population (7,532)
was age 65 or older[25]. Altogether, if we assume that these rates and demographics have
remained relatively stable and that incidence rates in the city are similar to
those in the county, then we can assume that 32% of of
seniors in Schenectady County reside within the city of Schenectady, and we can
estimate that the city annually experiences approximately 354 ED visits, 174
hospitalizations, and nearly 3 deaths due to falls among seniors.
The
United States Centers for Disease Control and Prevention (CDC) reports that the
average Medicare costs per fall are between $9,113 and $13,507 [26]. The average costs of a fall-related ED visit is
probably different than the average cost of a fall-related hospitalization.
However, if we apply the CDC’s average Medicare costs to our ED and
hospitalization estimates, then we can estimate that fall-related ED visits and
hospitalizations in seniors ages 65 and older in the city of Schenectady cost
between $4,811,664 and $7,131,696 annually.
The
Falls-HIT (Home Intervention Team) Program is a fall prevention intervention
that involves home visits by occupational therapists and supports home
modification to improve safety[27]. A study found that the Falls-HIT Program reduced
the fall rate among participants by 31% [28]. Based on the previous cost estimates, if the
Falls-HIT Program were implemented with similar efficacy throughout
Schenectady, then it could produce between $1,491,615 and $2,210,825 in annual
savings through fall prevention.
These
preliminary estimates suggest that fall prevention could be a viable use case
for SIBs. Moving forward, more investigation would be necessary to better
understand fall prevalence within the city, associated costs, as well as the
scalability and efficacy of a fall prevention program in Schenectady. Fall
prevention produces direct savings through averted healthcare costs, and so a
fall prevention SIB could be well suited for facilitating a partnership between
public and private health insurance providers. Appropriate outcome metrics for
this type of SIB would be hospitalization, ED visits, and mortality due to
falls per 10,000 population age 65 and older in the city of Schenectady.
IX.
SIB Case: Type 2 Diabetes
Type
2 diabetes is epidemic in New York State[29]. Results from the UMatter
Schenectady Survey indicate that the prevalence in the city is high:
• 11.6% of all UMatter
respondents reported that they had been diagnosed with type 2 diabetes by a
health professional[30].
• Among non-diabetic UMatter
respondents, 13.9% reported that they had been diagnosed with pre-diabetes by a
health professional[31].
Type
2 diabetes is an expensive chronic disease to manage. The average annual cost
of healthcare for a person with diabetes is $11,744, of which $6,649 is
attributable to diabetes[32]. In contrast, the average annual cost of healthcare for a
non-diabetic is $2,560 [33]. All respondents in the UMatter survey
were ages 18 and older; the US Census estimates that in 2012, the city’s 18 and
older population was 49,954 [34]. From the UMatter
findings, we can estimate that in the city’s 18 and older population, there are
approximately 5,794 people with type 2 diabetes, and 6,138 people with
pre-diabetes. By this, we can further estimate that among adults in the city of
Schenectady, annual medical expenditures attributable to type 2 diabetes amount
to approximately $38,524,306.
The
National Diabetes Prevention Program is an evidence based intervention that reduces
the risk of developing type 2 diabetes by 58% in people with pre-diabetes[35]. The program is available in Schenectady[36], but the capacity is restricted by maximum class
sizes and the availability of personnel and facilities. A SIB could be effective
at scaling the program. If the National Diabetes Prevention Program were
expanded in Schenectady, it could prevent up to 3,560 people with pre-diabetes
from developing type 2 diabetes, and would thereby generate up to $26,775,124
in annual savings through averted healthcare expenditures attributable to
diabetes.
The
cost of diabetes and efficacy of preventive intervention together suggest that
a diabetes-focused SIB could be effective in Schenectady. More investigation
should be conducted to measure pre-diabetes prevalence, and to more precisely
estimate the scalability and efficacy of the National Diabetes Prevention
program in Schenectady. An appropriate outcome metric for this SIB could be
type 2 diabetes incidence in the city of Schenectady.
X.
SIB Case: Tobacco Smoking
According
to the CDC, tobacco use is the leading cause of preventable death in the United
States, and life expectancy is 10 years shorter for people who smoke[37]. The UMatter survey
found that 37.1% of respondents are current smokers; all respondents in the
survey were ages 18 and older[38]. In 2012, the city of Schenectady had 18 and
older population of 49,954 [39]. Altogether, we can estimate that there are
approximately 18,532 adult smokers in Schenectady.
Based
on data from a 2008 CDC Morbidity and Mortality Weekly Report, the American
Lung Association estimated that smoking cost an average of $4,260 per adult
smoker in lost productivity and direct healthcare expenditures in 2004 [40]. If we assume that the cost of smoking has
remained relatively constant since 2004, then the American Lung Associations
estimation suggests that the cost of adult smoking in Schenectady is
approximately $78,946,320 annually.
The
UMatter Schenectady Survey found that although
smoking prevalence in Schenectady is high, there is also great interest in
cessation. The survey found that 49.2% of current smokers have tried to quit
within the last year; out of these respondents, 65.2% reported that they
attempted to quit without assistance by going ‘cold turkey’[41]. For many smokers, assisted quit programs can be
more effective. In a 2000 study, Zhu et al. found that smokers who tried
to quit with assistance (15.2%) were more successful than those who tried to
quit unassisted (7.0%) [42].
The
Butt Stops Here is a one-on-one counseling program that, cooperatively, is
hosted in Schenectady at Ellis Hospital and run by Seton Health of the
Albany-based St. Peter’s Health Partners. The program achieves a 30% quit rate[43]. With greater access to capital and a scaled up
referral system, The Butt Stops Here could increase its service capacity. A SIB
could be an effective solution. Up to $11,653,289 could be saved annually by
extending The Butt Stops Here to adult smokers in Schenectady who have tried to
quit in the last year; up to $23,685,548 in annual savings could be achieved by
extending the program to all of Schenectady’s adult smokers.
A
SIB for smoking cessation and prevention in Schenectady could produce
significant cost savings by scaling new or existing programs. Smoking
prevalence, as measured by the UMatter Schenectady
Survey or other public health surveillance systems, would be an appropriate
outcome metric for evaluating the success of the intervention.
XI.
Discussion and Recommendations
The
evidence-based interventions outlined in the preceding sections can improve
Schenectady’s public health and generate savings:
SIB Use Case Estimated Total Savings
• Asthma prevention $5.30
to $14.00 per dollar invested
SIB Use Case Estimated Annual Savings
• Fall prevention among seniors Between
$1,491,615 and $2,210,825
• Type 2 diabetes prevention Approximately
$26,775,124
• Tobacco Smoking cessation Approximately
$23,685,548
I
recommend that Schenectady explore these, and other opportunities for
developing public health-focused SIBs. I also recommend that the city work
collaboratively to develop SIBs in partnership with New York State and with
private health insurance companies.
Importantly,
the SIB use cases in this report only present preliminary estimates of maximum
possible cost savings. The estimates do not account for costs of developing and
deploying SIBs, such as contracting with intermediaries and compensating
investors. Further analysis should be conducted for each use case in order to
better estimate prevalence, incidence, and costs attributable to morbidity and
mortality. In addition, the interventions to be considered should be
evidence-based, ethical, and they should be chosen on the basis of feasibility,
scalability, and probable efficacy in Schenectady.
Schenectady
is well suited for developing and deploying a health impact bond. It is the
only city in upstate New York’s geographically second smallest county; it is
served by a county health department, a single acute care hospital with a
formal outpatient campus, and a Medicaid Health Home; and Schenectady is
located in a region with significant academic resources. Schenectady can draw
on services and expertise from an organized community-wide coalition of health
and community service providers; and, the majority of non-government health
insurance in Schenectady is provided by two regional not-for-profit health
plans.
SIBs
are a relatively new invention, and the regulatory framework that governs them
is still developing at the state and federal levels. The two SIB pilots now
underway in New York City and New York State demonstrate that SIBs can legally
be developed in New York’s largest city, and within a designated state program.
Schenectady is generally subject to the more restrictive provisions of the
state’s Local Finance Law, and therefore should consult with legal experts and
perhaps consider requesting special state legislation.
As
the adoption of health impact bonds continues, I hope that accountable care
organizations, patient-centered medical homes, and employers will join
governments and health insurance providers as partners in health impact bond
development. In the future, health impact bonds could become major drivers of
investment into public health. Furthermore, they could create economic
incentives for deploying resources for addressing neglected public health
challenges that before were unprofitable.
I expect that SIBs will grow tremendously as an asset class. I predict that in the future, SIBs will be able to raise investor capital through formal initial public offerings, and I expect that SIB shares will be traded on dedicated exchanges as dividend-yielding securities. This could perhaps give rise to the creation of ‘exchange-traded SIB funds’ (ETSFs) that would enable investors to make diversified or sector-specific impact investments across multiple SIBs. In the future, it would be interesting to see the first ever ‘immunization ETSF’, ‘clean water ETSF’, ’cancer prevention ETSF’, ’pollution reduction ETSF’, or ’New York State ETSF’.
[1] MPH Candidate, Epidemiology; University at Albany, School of Public
Health.
Email: imichaels@albany.edu.
[2] Bloomberg, M. R. (2012, August 02). Bringing social impact bonds to New York City. Retrieved from http://www.nyc.gov/html/om/pdf/2012/sib_media_presentation_080212.pdf
[3] Massachusetts Executive Office of Administration and Finance, (2012). Massachusetts first state in the nation to announce initial successful bidders for ‘pay for success’ contracts. Retrieved from website: http://www.mass.gov/anf/press-releases/fy2013/massachusetts-first-state-in-the-nation-to-announce-ini.html
[4] Fact sheet: the Utah High Quality Preschool Program America’s first social impact bond targeting early childhood education. (n.d.). Retrieved from http://www.goldmansachs.com/what-we-do/investing-and-lending/urban-investments/case-studies/impact-bond-slc-multimedia/fact-sheet-pdf.pdf
[5] Badawy, M. (2012, October 19). California city seeks to cut asthma rate via bond issue. Retrieved from http://www.reuters.com/article/2012/10/19/us-investing-impactbonds-health-idUSBRE89I0U120121019
[6] Disley, E., Rubin, J., Scraggs, E., Burrowes, N., & Culley, D. U.K. Ministry of Justice, (2011). Lessons learned from the planning and early implementation of the social impact bond at HMP Peterborough. Retrieved from website: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/217375/social-impact-bond-hmp-peterborough.pdf
[7] Goldberg, S. H. (2013, January). Do sibs qualify for the Community Reinvestment Act? oh, yeah. SIB TRIB, (2), 14. Retrieved from http://payforsuccess.org/sites/default/files/sib_trib_no._2.pdf
[8] ibid.
[9] GS social impact fund. (n.d.). Retrieved from http://www.goldmansachs.com/our-thinking/focus-on/impact-investing/touts/fact-sheet.pdf
[10] Morgan Stanley establishes institute for sustainable investing. (2013, November 1). Retrieved from http://www.morganstanley.com/about/press/articles/a2ea84d4-931a-4ae3-8dbd-c42f3a50cce0.html
[11] Institute for Sustainable Investing. (n.d.). Retrieved from http://www.morganstanley.com/sustainableinvesting/
[12] Eddy, M. (2012, September). Scaling tuberculosis treatment through a social impact bond. Instiglio, 5. Retrieved from http://www.instiglio.org/pub/Instiglio%20White%20Paper%20-%20Tuberculosis%20Social%20Impact%20Bond.pdf
[13] U.S. Census Bureau. (2013, December 13). State & county Quickfacts: Schenectady County, N.Y. Retrieved January 25, 2007, from http://quickfacts.census.gov/qfd/states/36/3665508.html
[14] Pratt, D., & Buckenmeyer, E. (2013, November 15). 2013 community health needs assessment and community action plan: a consolidated, multi-agency, community-wide plan for action to improve the health of people in Schenectady, New York. Schenectady Coalition for a Healthy Community, Retrieved from http://www.schenectadychamber.org/files/814.pdf
[15] New York State Department of Health, Center for Community Health. (2009). New York State asthma surveillance summary report. Retrieved from website: http://www.health.ny.gov/statistics/ny_asthma/pdf/2009_asthma_surveillance_summary_report.pdf
[16] ibid.
[17] U.S. Census Bureau. (2013, December 13). State & county Quickfacts: Schenectady (city), N.Y. Retrieved January 25, 2007, from http://quickfacts.census.gov/qfd/states/36/3665508.html
[18] U.S. Census Bureau, State & county Quickfacts: Schenectady County, N.Y.
[19] New York State Department of Health, Center for Community Health, Asthma surveillance summary report.
[20] Jacobs, D. E., & Baeder, A. (2009). Housing interventions and health: a review of the evidence. National Center for Healthy Housing, Retrieved from http://www.nchh.org/LinkClick.aspx?fileticket=2lvaEDNBIdU=&tabid=229
[21] New York State Department of Health, Injury Prevention Program. (2010). Incidence of unintentional fall injuries, ages 65+ emergency department (ed) visits new york state residents, 2006-2008. Retrieved from website: http://www.health.ny.gov/statistics/prevention/injury_prevention/docs/2006_2008_falls_ed65 county.pdf
[22] New York State Department of Health, Injury Prevention Program. (2010). Incidence of unintentional fall injuries, ages 65 hospitalizations new york state residents, 2006-2008. Retrieved from website: http://www.health.ny.gov/statistics/prevention/injury_prevention/docs/2006_2008_falls_hospital65 county.pdf
[23] New York State Department of Health, Injury Prevention Program. (2010). Incidence of unintentional fall injuries, ages 65 deaths new york state residents, 2006-2008. Retrieved from website: http://www.health.ny.gov/statistics/prevention/injury_prevention/docs/2006_2008_falls_deaths65 counties.pdf
[24] U.S. Census Bureau, State & county Quickfacts: Schenectady (county), N.Y.
[25] U.S. Census Bureau, State & county Quickfacts: Schenectady (city), N.Y.
[26] U.S. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. (2013). Cost of falls among older adults. Retrieved from website: http://www.cdc.gov/homeandrecreationalsafety/falls/fallcost.html
[27] Stevens, J. A. U.S. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. (2010). A CDC compendium of effective fall interventions: what works for community-dwelling older adults, 2nd edition. Retrieved from website: http://www.cdc.gov/homeandrecreationalsafety/pdf/cdc_falls_compendium_lowres.pdf
[28] ibid.
[29] New York State Department of Health, Division of Chronic Disease and Injury Prevention. (2011). Dual epidemics of diabetes and obesity are on the rise among New York State adults. Retrieved from website: http://www.health.ny.gov/statistics/prevention/injury_prevention/information_for_action/docs/2011-4_ifa_report.pdf
[30] Pratt, D., & Buckenmeyer, E., “2013 community health needs assessment and community action plan”.
[31] ibid.
[32] Dall, T., Edge Mann, S., Zhang, Y., Martin, J., Chen, Y., & Hogan, P. (2008). Economic cost of diabetes in the U.S. in 2007. Diabetes Care, 31(3), doi: 10.2337/dc08-9017
[33] New York State Department of Health, (2012). Diabetes. Retrieved from website: http://www.health.ny.gov/diseases/conditions/diabetes/
[34] U.S. Census Bureau, State & county Quickfacts: Schenectady (city), N.Y.
[35] U.S. Centers for Disease Control and Prevention, (2013). National Diabetes Prevention Program. Retrieved from website: http://www.cdc.gov/diabetes/prevention/about.htm
[36] YMCA diabetes prevention program. (n.d.). Retrieved from http://www.cdymca.org/healthyliving/diabetes.aspx
[37] U.S. Centers for Disease Control and Prevention, (2013). Tobacco-related mortality. Retrieved from website: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/tobacco_related_mortality/index.htm
[38] Pratt, D., & Buckenmeyer, E., “2013 community health needs assessment and community action plan”.
[39] U.S. Census Bureau, State & county Quickfacts: Schenectady (city), N.Y.
[40] American Lung Association, (n.d.). Smoking. Retrieved from website: http://www.lung.org/stop-smoking/about-smoking/health-effects/smoking.html
[41] Pratt, D., & Buckenmeyer, E., “2013 community health needs assessment and community action plan”.
[42] Zhu, S., Melcer, T., Sun, J., Rosbrook, B., & Pierce, J. (2000). Smoking cessation with and without assistance: a population-based analysis. American Journal of Preventive Medicine, 18(4), 305-11. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10788733
[43] ‘The Butt Stops Here’ smoking cessation Troy support group. (2010, June 28). Retrieved from http://www.setonhealth.org/news_events/event_detail.cfm?ID=286